ABOUT OUR INDUSTRY
About PCMA
The Pharmaceutical Care Management Association (PCMA) is the national association representing America’s pharmacy benefit managers (PBMs). PBMs administer prescription drug plans for more than 266 million Americans who have health coverage from a variety of sponsors. PCMA continues to lead the effort in promoting PBMs and the proven tools they utilize, which are recognized by consumers, employers, policymakers, and others as key drivers in lowering prescription drug costs, increasing access, and improving outcomes.
PBMs are Committed to Helping Patients
Pharmacy Benefit Managers (PBMs) are your advocates in the health care system, working to lower prescription drug costs for patients and payers across the country.
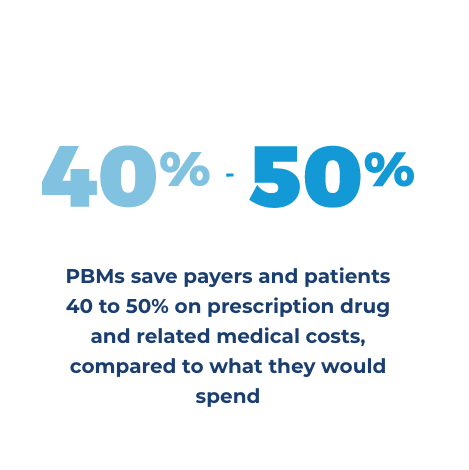
PBMs administer prescription drug plans for more than 266 million Americans who have health insurance from a variety of sponsors including: commercial health plans, self-insured employer plans, union plans, Medicare Part D plans, the Federal Employees Health Benefits Program (FEHBP), state government employee plans, managed Medicaid plans, and others. PBMs will save health plan sponsors and consumers more than $1 trillion on prescription over 10 years.
HOW PBMs WORK FOR YOU
Virtually all – 99.6% of prescription drug rebates PBMs negotiated with drug manufacturers in Medicare Part D are passed through to drug plan sponsors and used to lower costs for Medicare beneficiaries, according to the U.S. Government Accountability Office (GAO).


When PBMs
Succeed You Save
- PBMs offer home delivery of medications and creating select networks of more affordable pharmacies.
- PBMs encourage the use of generics and more affordable brand medications.
- PBMs negotiate rebates from drug manufacturers and discounts from drugstores.
- PBMs manage high-cost specialty medications.
- PBMs reduce waste and improve adherence.
- More than 9 in 10 employers are satisfied with their PBM.
- According to a poll of employers, over four-fifths say their company’s contract with its PBM is transparent.
The vast majority of employers
say that PBM programs are
effective at reducing drug costs
for their organization.
See how much PBM tools could save
in your state over the next
10 years at OnYourRxSide
PBMs Will Save Health Plan Sponsors
and Consumers More than $1 Trillion on Prescription Drugs
PBMs Support Policies to
Lower Drug Costs and
Increase Quality of Care
Top 20 Federal Solutions for High Drug Costs
- Eliminate anticompetitive “pay-for-delay” agreements. Patent settlements, or “pay-for-delay” agreements, allow brand name drug and biologic patent holders to pay potential competitors to delay market entry or not produce a competing generic drug or biosimilar.
- End orphan drug exclusivity abuses. Orphan exclusivity periods should apply only to those prescription drugs originally approved by the Food & Drug Administration (FDA) under an orphan indication and only for the orphan indication itself.
- Revise innovator biologic exclusivity to seven years. Seven years (reduced from 12 years under current law) of market exclusivity would provide sufficient return for manufacturers while speeding competitor biosimilars to market to promote affordability and access.
- Allow for FDA accelerated approval of me-too brands. Accelerated review is granted by the FDA to new drug applications that address “unmet need,” the criterion for which should be updated to account for the economic need for competition to lower prices.
- Promote uptake of biosimilars and interchangeables. Policies should encourage market entry of biosimilars, rather than erect unnecessary barriers, including barriers to achieving interchangeability and therapeutic substitution. Uptake also can be supported by requiring use of a common billing code to pay for a reference biologic and its biosimilars.
- Promote broader adoption of value-based purchasing, including by modernizing and better aligning the Stark Law and Anti-Kickback Statute to promote value-based care and clarifying value- and outcomes-based arrangements for the purposes of Medicaid Best Price.
- Eliminate the tax deductibility of direct-to-consumer (DTC) prescription drug advertising. While DTC drug ads may encourage some to seek care, they also may encourage costlier and unnecessary forms of care—with the result being higher health care costs for all.
- Ensure smooth implementation of real-time benefit tools (RTBTs) in Part D and empower prescribers to inform patients of cost-effective, therapeutically equivalent medications by extending RTBT solutions to Medicaid and the Health Insurance Marketplace.
- Promote wider adoption of electronic prescribing (eRx), including by requiring eRx for all prescriptions (not just controlled substances in Medicare), subject to limited exceptions to decrease fraud and diversion and increase patient access and safety.
- Allow select exclusions in protected classes. The Medicare Payment Advisory Commission (MedPAC) recommends applying objective criteria to make select exclusions of protected classes (e.g., classes where the Centers for Medicare & Medicaid Services (CMS) and MEDPAC have identified the availability of many treatment options) to allow plan sponsors to more directly manage prescription drugs.
- Promote availability of biosimilars in protected classes by ensuring Part D plans have the flexibility to cover the biosimilar or the innovator product – but not require coverage of both – where there is a biosimilar in the class.
- Modify the two drugs per-class requirement. The current requirement that Part D plans cover two drugs per class is outmoded. Instead, modifying the requirement by requiring plans to ensure access to therapies based on conditions or disease states would reduce costs without sacrificing access to needed drugs.
- Encourage innovative Part D benefit design to lower costs and improve access to care by allowing Part D plan sponsors to offer additional plans, including designs that offer enrollees more options to use money-saving and convenient home delivery.
- Repeal any willing pharmacy provisions. Requirements that all pharmacies be included in Part D networks drives up costs and are unnecessary, given CMS network adequacy requirements. Congress should repeal the provision. As Congress considers such action, CMS could evaluate allowing plan sponsors the ability to offer a narrower network plan option.
- Give Part D plans meaningful access to Part A and B claims data. To coordinate care and make the best coverage decisions for beneficiaries, Part D plans need to be able to use medical data as well as prescription data. Legislative changes allowing use of these data for this purpose also would advance indication-based formularies and decrease prescriber burden.
- Encourage the use of lower-cost drugs in Medicare Part D by allowing CMS to modify cost sharing for Low-Income Subsidy beneficiaries to establish stronger incentives to select generic and low-cost brand drugs (e.g., zero-dollar copayments), with increasing levels of copayments for less cost-effective therapeutic options.
- Build on existing efforts to apply Part D tools to Part B drugs. Adding Part D tools (e.g., value-based formularies, manufacturer negotiation, prior authorization, and step-therapy) to Medicare fee-for-service and building on efforts in Medicare Advantage to allow step therapy for Part B drugs would make drugs more affordable on the medical side of the Medicare benefit.
- Eliminate the cap on the inflationary penalty in the Medicaid Drug Rebate Program to discourage drug manufacturers from imposing excessive increases to list prices.
- Permit states the same tools available to commercial and Medicare Part D plans to limit coverage of drugs for which there is inadequate evidence of clinical effectiveness or ample competition of therapeutic alternatives. A waiver of section 1902(a)(54) – beyond the adult expansion population – would enable states to adopt private-sector formulary management techniques into their Medicaid programs.
- Allow states flexibility in their pharmacy payment approach. States are required to use pharmacy reimbursement methodologies in accordance with the definition of Actual Acquisition Cost, leading to dispensing fees up to $12 per prescription. This is incongruent with Medicaid managed care and efforts to promote value-based purchasing of pharmacy care.