The core mission of pharmacy benefit managers (PBMs) is to reduce prescription drug costs for health plan sponsors so that consumers have affordable access to needed prescription drugs. PBMs offer a variety of services to their health-plan-sponsor clients and patients that improve prescription adherence, reduce medication errors, and manage drug costs.
The proposed Mississippi legislation will seriously undermine the ability of PBMs to control drug costs, and as a result drug spending in Mississippi will soar. Although many of the provisions are vague and subject to various interpretations, enacting just the three bill provisions discussed below could cost the state of Mississippi up to $100 million in excess drug spending in the first year alone, and $1.2 billion over the next 10 years.
1. Section 4. 73-21-156 Mandated Changes to PBM MAC Lists: requiring PBMs to change their Maximum Allowable Cost (MAC) lists would remove incentives for pharmacies to purchase the most cost-effective generic drugs. Generic drugs comprise 90% of all prescription drug fills, inefficient purchasing of these would cause drug costs to soar. This type of “guaranteed profit” legislation undermines competitive market dynamics, is a giveaway to pharmacy special interests, and would harm Mississippi employers, unions, and patients.¹
2. Section 5. 73-21-157 Elimination of PBM pharmacy accreditation standards: forcing PBMs to eliminate their accreditation standards potentially puts patients at risk, and creates a de facto Any Willing Provider (AWP) environment with state pharmacies. Any Willing Provider mandates increase costs for patients as they reduce cost-efficient specialty pharmacy usage and pharmacies that previously provided the deepest discounts no longer will as they can no longer count on getting added volume in exchange.
3. Section 7. 73-21-161 Limiting PBM Ability to Create Pharmacy Networks: PBMs create networks of pharmacies that offer savings to clients and beneficiaries. Creation of these pharmacy networks are popular with employers and help save money on drug costs. Nationally, 76% of employers report using some type of narrowed pharmacy network, and their employees can save 38% out of pocket using the in-network pharmacies versus out-of-network pharmacies.²
Projected 10-Year Increases in Prescription Drug Spending In Mississippi Insurance Markets Due to Adopting Proposed Policies, 2021–2030 (Millions)
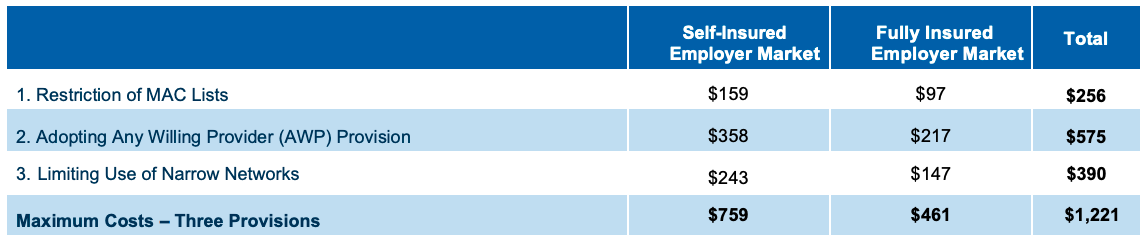
Methodology: The methodology used to create the restriction of MAC list estimates was that used by Visante in their January 2015 paper “Proposed MAC Legislation May Increase Costs of Affected Generic Drugs By More Than 50 Percent.” Estimated impact used in creation of projections as 1.5%. The methodology used to create the AWP and Narrow Networks cost projections was that used by Visante in their April 2020 paper “Increased Costs Associated With Proposed State Legislation Impacting PBM Tools.” The AWP cost impact only applies to prescriptions filled through specialty pharmacies. The narrow networks provision estimate includes impact to prescriptions filled through retail pharmacies and mail order pharmacies.
1 David A. Hyman, 2016. “The Adverse Consequences of Mandating Reimbursement of Pharmacies Based on Their Invoiced Drug Acquisition Costs.”
2 PBMI, 2019. “2018 Trends in Drug Benefit Design.


