Morning Consult: Congress Should Act Quickly to Permanently Repeal the Rebate Rule
April 12, 2021
While Congress and the Biden administration, as well as stakeholders across the prescription drug supply chain, examine policy options for addressing high drug prices, pharmacy benefit managers continue…
Keep Reading >
PCMA Launches New Campaign Aimed At Repealing the Medicare Prescription Drug Rebate Rule
March 1, 2021
(Washington, D.C.) — The Pharmaceutical Care Management Association (PCMA) unveiled a new campaign commending the Biden Administration for delaying the Medicare prescription drug rebate rule…
Keep Reading >
Rebate Rule Effective Date Postponed to 2023
January 30, 2021
(Washington, D.C.) — In response to litigation brought by the Pharmaceutical Care Management Association (PCMA) challenging the Medicare Part D rebate…
Keep Reading >
The Hill: The path forward for the Biden administration: Lowering drug costs without raising premiums for seniors
January 27, 2021
The new Biden administration has started off strong, taking a thoughtful approach to any number of critical health care issues…
Keep Reading >
PCMA Files Motion to Vacate Effective Date for Rebate Rule
January 26, 2021
(Washington, D.C.) — The Pharmaceutical Care Management Association (PCMA) has filed a motion for summary judgment to vacate the effective…
Keep Reading >
PCMA Federal Policy Priorities: 21 Policies to Reduce Prescription Drug Costs in 2021
January 14, 2021
(Washington, D.C.) — The Pharmaceutical Care Management Association (PCMA) today issued 21 policy solutions supported by America’s pharmacy benefit managers (PBMs) aimed at reducing prescription…
Keep Reading >
PCMA Files Lawsuit Challenging Rebate Rule
January 12, 2021
(Washington, D.C.) — The Pharmaceutical Care Management Association (PCMA) today filed a lawsuit challenging the Trump Administration’s rebate rule. PCMA’s…
Keep Reading >
PCMA: Pharmacy Benefit Managers Ready to Work with the New Administration to Lower Prescription Costs
November 07, 2020
Keep Reading >
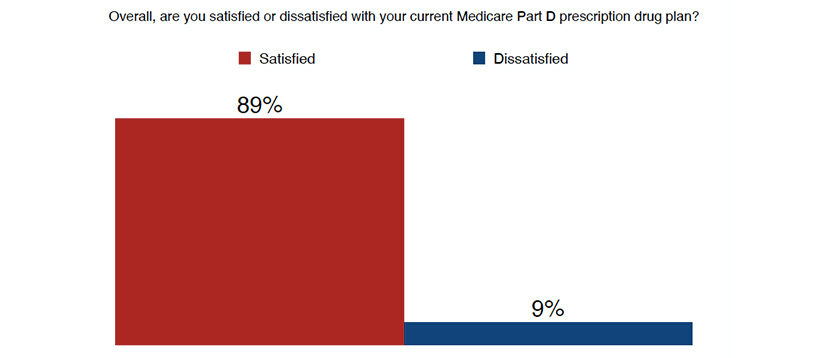
Pharmacy Benefit Managers Continue to Keep Medicare Part D Premiums Affordable
October 16, 2020
(Washington, D.C.) — Pharmaceutical Care Management Association President and CEO JC Scott issued the following statement on the open enrollment season for the…
Keep Reading >
New Report Confirms Proposed “Rebate Rule” Would Raise Medicare Premiums and Taxpayer Costs
September 08, 2020
(Washington, D.C.) — A new report, “Negative Economic Impact of Restricting Rebates in Medicare Part D,” by Alex Brill of…
Keep Reading >